Understanding Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
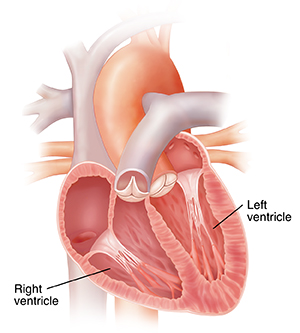
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a disease of the heart muscle. It used to be called arrhythmogenic right ventricular dysplasia (ARVD). ARVC is a rare genetic disease. It usually starts between ages 10 and 50. With this genetic defect, proteins that usually hold the heart muscle cells together don't develop normally. Because of this, the muscle cells can detach and die. These cells are then replaced by fatty fibrous tissue in the lower chambers of the heart, often the right ventricle. This interrupts normal electrical signals. The condition is characterized by irregular and possibly dangerous heart rhythms (arrhythmias) in the ventricles. The heart also becomes weaker over time. This can lead to heart failure. The disease can be very mild in some people, and severe in others.
How to say it
ar-RIHTH-moh-jehn-ik
RIT
vehn-TRIHK-yoo-ler
KAR-dee-oh-mi-AH-puh-thee
What happens in ARVC?
ARVC most often starts in a small part of the right ventricle. Over time, the disease slowly affects more of the right ventricle. Sometimes the left ventricle may be affected too. This can lead to abnormal heart rhythms. It can sometimes cause sudden death. Over time, the heart can’t pump as much blood as it normally would. Blood backs up in the circulatory system. This causes fluid to build up in the legs and sometimes in the lungs. This is called heart failure. This can lead to many symptoms, including shortness of breath and fatigue.
What causes ARVC?
ARVC results from an abnormal gene. The gene causes normal heart tissue to be replaced with fatty or fibrous tissue. Most cases of ARVC are from an abnormal gene from only one parent. But even if you have an abnormal gene, you may not have any major symptoms from ARVC. Researchers are working to understand what makes the disease more or less severe in some people.
If someone in your family has ARVC, you may be able to use genetic testing to see if you have the abnormal gene. Anyone with the abnormal gene should see their health care provider for regular checkups.
Symptoms of ARVC
Some people with ARVC show no symptoms. And others may have more severe symptoms. Symptoms of ARVC tend to get worse over time as the disease affects more of the heart. The most common symptoms are:
Other symptoms may include:
-
Shortness of breath with exertion.
-
Shortness of breath when lying down.
-
Chest pain.
-
Fatigue.
-
Swelling in the legs and other areas.
-
Persistent cough.
-
Sudden death because of an abnormal heart rhythm.
Heart palpitations and fainting are common early dangerous symptoms. In some cases, sudden death may be the first symptom of ARVC. The other symptoms linked with heart failure tend to occur over time.
Diagnosing ARVC
ARVC can be hard to diagnose. Your health care provider will ask about your past health, family health history, and symptoms. They will give you a physical exam. You will likely need to see a cardiologist. You may need tests, such as:
-
Electrocardiogram (ECG) to check the heart rhythm.
-
Continuous portable ECG monitoring to check heart rhythms over time. This might be a Holter or event monitor.
-
Signal-averaged ECG to check how likely you are to have heart rhythm problems.
-
Echocardiogram to look at blood flow in the heart and the heart’s motion.
-
Exercise ECG testing to check the heart rhythm during exercise.
-
Cardiac MRI to look at the heart anatomy and heart wall motion.
-
Angiography with catheterization, to look at the vessels and chambers in the heart.
-
Heart biopsy to look at the heart tissue in more detail.
-
Electrophysiology study to look at your heart's electrical system and to assess the risk of dangerous heart rhythm.
Genetic testing can confirm the diagnosis, but usually this is not needed. It can be helpful in cases in which the diagnosis is not clear. It can also be helpful when screening relatives after the genetic defect has been identified.
Treatment for ARVC
The main goals of treatment are to slow disease progression, reduce the occurrence of ventricular arrhythmias, and prevent sudden cardiac death. Treatment may include:
-
Not doing any high-intensity or endurance activities.
-
Taking medicines, such as beta-blockers or antiarrhythmics.
-
Getting an implantable cardioverter-defibrillator.
-
Having radiofrequency ablation done.
-
Having a heart transplant (rare).
Your health care provider will help you determine which choices are best for you. Discuss all your questions and concerns with your provider to make sure that you understand your diagnosis and your treatment choices.